My fiancé and I were at the gym today, about to begin our workout when she came to me with a question. She told me that she had been having pain in her left hip that started a week ago. She said it feels like her hip is jammed and gives her sharp pain when squatting. She thought it was just muscular tension at first, but after a week the problem was still not getting better. She began worrying when she noticed that it was not only feeling tight, but it was also effecting her mobility. I should mention that by trade, she is an aerial silks performer and professional dancer, so loss of hip mobility for her is simply not an option. That being said, I thought this would be a good opportunity to not only help her fix this, but to also use the situation as a means to educate on how I work through a situation like this.
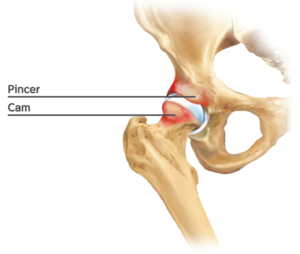
Table of Contents
History: For a patient with pain in the groin and hip area
In any situation like this, it is good to start with a history. If you find yourself at any doctors office that skips past this crucial step, I’ll advise you to respectfully find your way out of that office.
A 27 year old female presents with left sided pain in the groin and hip area with loss of mobility. She says the pain has been occurring for about 1 week and has gotten worse since that time. She says the left hip feels like it is jammed and that it looks and feels like her hips are uneven when squatting. She also states that when squatting she gets a muscular stretching type pain and in certain positions it feels sharp and shooting.
I will note that there is no history of trauma, appears to be no swelling, no night pain, and no neurological symptoms. Her gait pattern remains normal and there appear to be no changes to balance, coordination or posture.
Examination:

Upon palpation she experiences sharp pain at the groin and hip area, specifically at the location of the hip flexor directly medial to the hip joint. No other pinpoint pain was produced with palpation. I always recommend seeking professional help in these cases, however, you can palpate around your own hip to find locations of tenderness.
During examination we performed the following tests.
- Straight leg raise
- Results: Negative. Within normal limits.
- Dermatome testing (in this case using a pinwheel for sharp sensation)
- Results: Within normal limits.
- Manual muscle testing
- Results: Within normal limits. Significant other findings: She felt “seizing/spasm with knee flexion and extension” directly anterior and medial of the hip joint.
| Grade | Criteria |
| 5 | Normal strength |
| 5- | Uncertain muscle weakness |
| 4+ | Ability to move through full range of motion and hold against strong pressure |
| 4 | Ability to move through full range of motion and hold against moderate pressure |
| 4- | Ability to move through full range of motion and hold against slight pressure |
| 3 | Ability to move through full range of motion and hold against gravity |
| 3- | Ability to move through partial range of motion against gravity |
| 2 | Ability to move through any range of motion only with gravity eliminated |
| 1 | A flicker of movement is seen or felt within the muscle |
| 0 | No contraction within the muscle is palpable |
| Lower Extremity Manual Muscle Testing | |||
| ACTION | MUSCLES | NERVES | NERVE ROOTS |
| Hip flexion | Iliopsoas | Femoral nerve and L1-L3 nerve roots | L1, L2, L3, L4 |
| Knee Extension | Quadriceps | Femoral Nerve | L2, L3, L4 |
| Knee Flexion | Hamstrings | Sciatice Nerve | L5, S1, S2 |
| Hip Abduction | Gluteus medius and minimus, tensor fasciae latae | Superior Gluteal Nerve | L4, L5, S1 |
| Hip Adduction | Obturator externus, adductor longus, adductor magnus, adductor brevis, gracilis | Obturator Nerve | L2, L3, L4 |
| Toe Dorsiflexion | Extensor hallucis longus, extensor digitorum longus | Deep Peroneal Nerve | L5, S1 |
| Foot Dorsiflexion | Tibialis anterior | Deep Peroneal Nerve | L4, L5 |
| Foot Plantar Flexion | Triceps surae (gastrocnemius and soleus) | Tibial Nerve | S1, S2 |
| Foot Eversion | Peroneus longus and brevis | Superficial peroneal nerve | L5, S1 |
| Foot Inversion | Tibialis posterior | Tibial nerve | L4, L5 |
| Note: When one nerve root is more important than others, it is shown in bold |
Orthopedic Tests to consider when dealing with pain in the groin and hip
- Thomas Test
- Result: Positive with pain at the distal insertion of the hip flexor muscle
- Trendelenburg Sign
- Result: Negative test
- FABER Test
- Result: Positive test with pain at anterior hip joint
- FADDIR test
- Result: Positive test with pain at anterior hip joint
- Ober’s Test
- Result: Negative
- Log Roll Test
- Result: Positive test with pain during internal rotation and decrease range of motion during internal and external rotation
- Stinchfield Test
- Results: Negative
- Ely’s Test
- Result: Negative
Differential Diagnosis for groin and hip pain
To begin to determine the actual diagnosis of the problem, we first need to think about all of the possibilities that could be causing the symptoms. Then, we begin to rule them out one by one until we have an answer or a most likely cause. Below, is my differential diagnosis relating to the history and examination that was performed. For the purpose of this discussion I have already ruled out certain causes and have listed them below.
- Primary differential diagnosis’ that have been ruled out:
- Orthopedic and rheumatological causes
- These differential would be certain types of arthritis, myelitis, dislocations, gout, and fractures.
- Hernias, aneurysms and benign lumps
- A palpatory examination was performed ruling out inguinal and femoral hernia, lymphadenopathies, lipomas and cysts as well as femoral artery pathologies.
- Malignant causes
- With the results of the history and physical examination as well as the patients age and health status the following malignant causes have been ruled out.
- Osteosarcoma
- Metastatic diseases
- With the results of the history and physical examination as well as the patients age and health status the following malignant causes have been ruled out.
- Miscellaneous Causes
- Renal calculus and iliopsoas abscess have been ruled out due to history and physical examination findings.
- Orthopedic and rheumatological causes
- Our working Differential Diagnosis
- Trochanteric Bursitis
- Iliotibial Band Syndrome
- Meralgia Parasthetica
- Avascular Necrosis
- Labral Tear
- Referral Pattern from lumbar spine or sacroiliac joint
- Hip Impingement / Femoro-acetabular impingement
- Strain/Tear of hip muscle
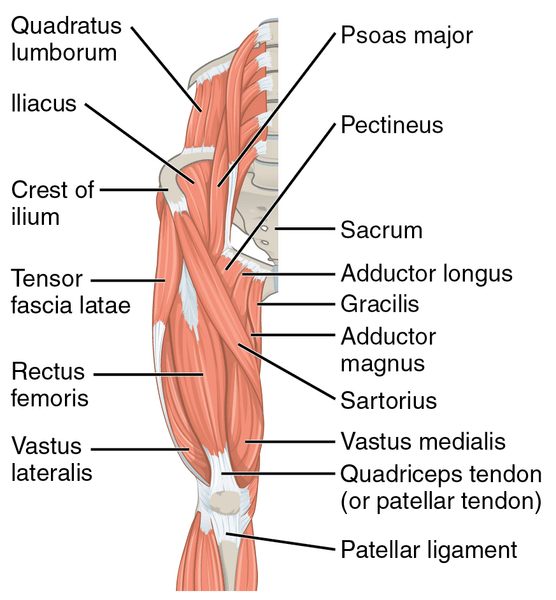
- Muscle of the hip flexor group
- Rectus femoris
- Iliacus
- Psoas
- Iliocapsularis
- Sartorius
- Pectineus
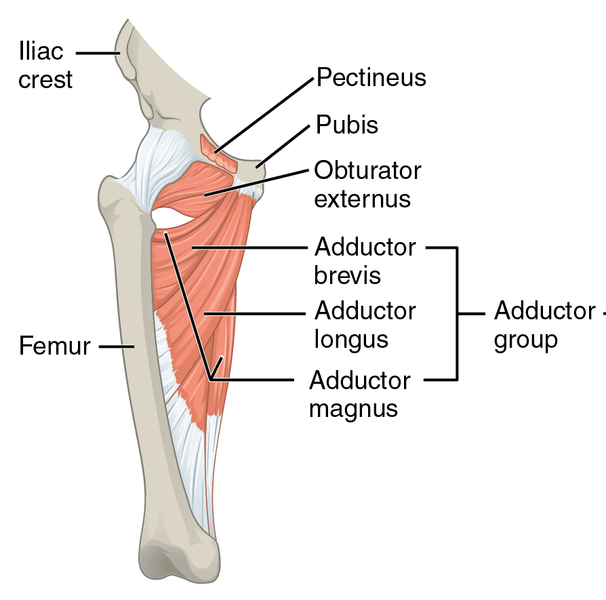
- Muscle of the adductor group
- Adductor longus
- Adductor brevis
- Adductor magnus
- Pectineus
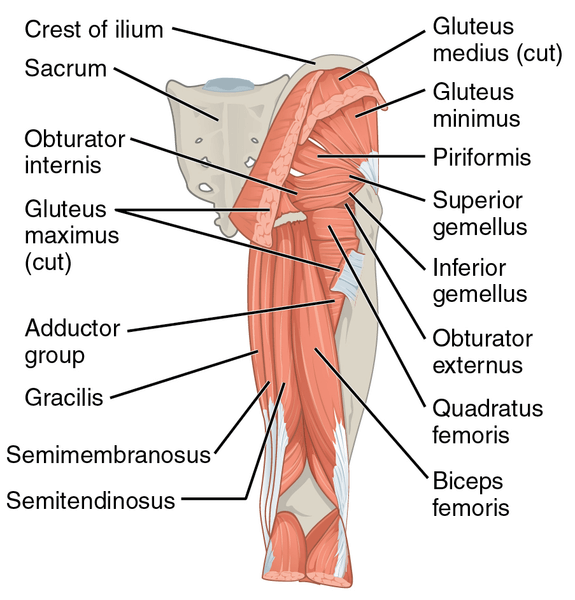
- Muscle of the abductor group
- Gluteus medius
- Gluteus minimus
- Tensor fasciae latae
- Piriformis
- Superior fibers of gluteus maximus
- Muscle of the hip extensor group
- Gluteus maximus
- Posterior head of adductor magnus
- Hamstrings
- Biceps femoris
- Semimembranosus
- Semitendinosus
- Muscle of the hip flexor group
Ruling out from our Differential Diagnosis
Because we can have multiple issues happening at the same time, it is not essential to rule every differential diagnosis out. Often times, we can have multiple issues occuring at the same time. There typically is a primary diagnosis that causes other types of issues. An example of this would be hip impingement with a secondary diagnosis of trochanteric bursitis. So, keep this in mind.
Due to our results of muscle and orthopedic testing, we know that hip flexion, knee flexion and knee extension caused reproduction of symptoms. Also, the only pain occurring is at the anterior aspect of the hip joint. Therefore, in my opinion, we can rule out pathologies involving the abductor and hip extensor groups.
Since we have no lower back or sacral/sacroiliac findings on our history or examination, we are also going to rule out referral patterns from the lower back and sacroiliac joint as well as meralgia paresthetica. These diagnosis’ would likely be cause by nerve root inflammation of the lumbar and sacral nerves. We also know that our neurological findings were not positive, likely indicating that we are not dealing with a diagnosis involving any nerve roots.
Avascular necrosis is still in our differential at this time, however, pain was not reproduced while walking, or running. We also know that there is no history of trauma and no history of blood diseases that we are aware of. The patient also has no history of steroid or excess alcohol use which can cause this type of diagnosis.
At this point we are left with a much smaller differential diagnosis.
After rule out, our current Differential Diagnosis is as follows:
- Trochanteric bursitis
- Labral Tear
- Hip/Femoroacetabular impingement
- Strain/Tear of hip muscle
- Muscle of the hip flexor group
- Rectus femoris
- Iliacus
- Psoas
- Iliocapsularis
- Sartorius
- Pectineus
- Muscle of the adductor group
- Adductor longus
- Adductor brevis
- Adductor magnus
- Pectineus
- Muscle of the hip flexor group
At this point we are also going to rule out a labral tear of the hip. Although this is still a possibility, due to our history on exam, I believe this to be a unlikely. A labral tear of this hip will usually present with not only pain, but clicking, instability, and locking sensations within the hip joint. Because she has none of these symptoms at the time, we are going to rule this out unless these symptoms become present at another point in time.
We are also going to rule out trochanteric bursitis at this time, because although we do have pinpoint tenderness upon palpation at the anterior aspect of the hip, we do not have pinpoint tenderness at the lateral aspect of the hip.
Working Diagnosis
Hip / Femoroacetabular Impingement
In this case, I believe we may be dealing with multiple issue. The first diagnosis is femoroacetabular impingement due to her pain and immobility in the position of hip flexion, adduction and internal rotation.
Strain of a muscle of the Hip Flexor and/or Adductor group (Pectineus)
Due to her pain being cause with certain muscular activation, I believe it is quite possible that we are dealing with a muscular strain as well. Looking back at the differential diagnosis, I began by trying to link the muscular action with the reproduction of pain. Unfortunately, I could not rule any of the muscles in the differential diagnosis in. At, this point, I muscle tested her in a few different positions. It turned out that she also experienced pain with hip adduction while the hip was externally rotated. This detail along with the direct location of tenderness on palpation led me to believe that we may be dealing with a mild pectineus adductor strain as well.
Treatment for Hip Impingement (Femoroacetabular Impingement)
Treatment for Hip Impingement should always begin with conservative and non-invasive methods such as Chiropractic care, Physical Therapy, or a combination of both. For individual where conservative care fails, surgical intervention may be required.
Ice: 15 – 20 minutes at a time. Allow at least 20-30 minutes between icing sessions and never ice directly on bare skin.
Protection: Avoid and alter activities that cause pain.
Banded Hip Mobilization for Hip Impingement
- Secure a heavy band to a wall or immovable object
- Begin exercise by placing band around the affected proximal femur as close to the groin as possible
- Walk out to tighten the band and assume a lunge position
- Begin internally rotating the femur and hold this position for 5-10 seconds
- Now externally rotate the femur and contract the gluteal muscles
- Repeat the internal and external sequence for 10 repetitions
Hip Range of motion exercises
Treatment for Muscle Strain
Ice: 15 – 20 minutes at a time. Allow at least 20-30 minutes between icing sessions and never ice directly on bare skin.
Protection: Avoid and alter activities that cause pain.
Elevate: Elevate the area to decrease swelling.
Avoid Stretching: Muscular strains should not be treated with active or passive stretching, stretching may worsen the injury and delay healing time.
Common treatments for Hip Flexor Strains
Advance Diagnosis if necessary
If conservative treatment fails, it may be necessary to seek advance imaging as well as more invasive measures. In some cases an MRI may be in order. And, if conservative care fails, surgical methods may be called for.